Your One-Stop Provider Credentialing Solution
Credentialing & Re-credentialing, Primary Source Verification and Continuous Monitoring for Assured Compliance
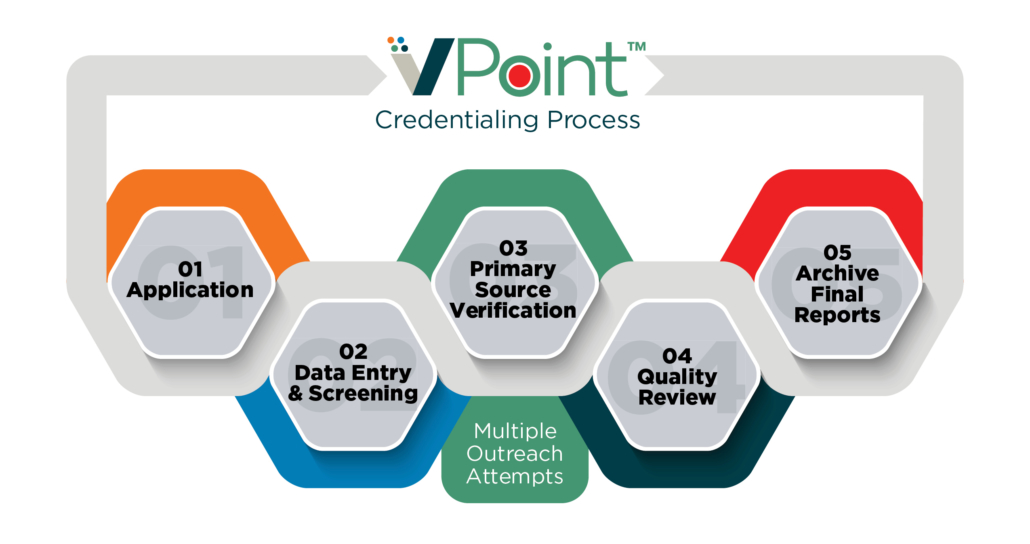
Vālenz® VPointTM is a comprehensive provider credentialing and continuous monitoring solution. Ideal for health systems, hospitals, medical groups, dentistry practices and health plans, VPoint offers excellence in credential verification to ensure compliance and quality of care. As a leading service provider for medical/dental credential verification – and as a key component of our commitment to delivering Validation, Integrity and Accuracy (VIA) for providers – VPoint is NCQA-certified and URAC-accredited.
Built from our CVO team’s extensive experience in provider credentialing, VPoint adapts to your unique needs while keeping pace with constant changes in healthcare and technology. The result is highly accurate and timely healthcare practitioner information, expert service and continuous monitoring that protects from fraud, waste and abuse as well as denials, appeals, unpaid claims, and penalties associated with deploying providers with licensing or disciplinary issues.
High Standards in Credentialing and Re-credentialing
VPoint’s team of experts follow the high industry standards of the Institute for Credentialing Excellence and these agencies and organizations:
National Committee for Quality Assurance (NCQA)
- License to Practice
- DEA or CDS Certification
- Education and Training
- Board Certification Status
- Work History
- Malpractice Claims History
- State Licensing Board Sanctions
- Medicare/Medicaid Sanctions
- Practitioner Application Processing
- Application and Attestation Content
- Ongoing Monitoring of Sanctions
Utilization Review Accreditation Commission (URAC)
- License to Practice (All states where Provider is practicing)
- DEA or CDS Certification
- Education and Training
- Board Certification Status
- Work History
- Malpractice Claims History
- State Licensing Board Sanctions
- Medicare/Medicaid Sanctions
- Practitioner Application Processing
- Application and Attestation Content
- Ongoing Monitoring of Sanctions
Centers for Medicare & Medicaid Services (CMS)
- License to Practice
- DEA or CDS Certification
- Education and Training
- Board Certification Status
- Work History
- Malpractice Claims History
- State Licensing Board Sanctions
- Medicare/Medicaid Sanctions
- Practitioner Application Processing
- Application and Attestation Content
- Ongoing Monitoring of Sanctions
- CMS Opt-Out
- SAM (EPLS)
- State OIG
The Joint Commission
- License to Practice (All states – current and past)
- ECFMG
- DEA or CDS Certification
- Education and Training
- Hospital Affiliations (current and past)
- Peer References
- Board Certification Status
- Malpractice Claims History
- State Licensing Board Sanctions
- Medicare/Medicaid Sanctions
- Practitioner Application Processing
- Application and Attestation Content
- Ongoing Monitoring of Sanctions
- CME
- Delineation of Privileges (DOP)
Accreditation Association for Ambulatory Health Care (AAAHC)
- License to Practice (current license)
- DEA
- Education and Training
- Board Certification Status
- Work History
- Primary Hospital
- Peer References
- Malpractice Claims History
- State Licensing Board Sanctions
- Medicare/Medicaid Sanctions
- Practitioner Application Processing
- Application and Attestation Content
- Ongoing Monitoring of Sanctions
- Delineation of Privileges (DOP)
Key Features & Benefits:
- Provider credentialing and re-credentialing
- Primary source verification
- Continuous monitoring of credentials and licensure
- Expert service and support from our team as a NCQA-certified, URAC-accredited CVO
- Provider application automation
- Immediate notification of provider sanctions and other license/disciplinary concerns
- Weekly electronic reporting
- Secure data exchange and storage
To further bolster your compliance management, VIA Provider Solutions includes a comprehensive compliance management solution to improve medical coding efficiency, reimbursement assurance, auditing toolsets, claims accuracy, provider credentialing, medical staff licensing and exclusion monitoring.