Simplify Healthcare
with the Vālenz Health® Platform
Self-Insurance Made Simple—Achieve Smarter, Better, Faster Healthcare

Your Platform for Elevating Healthcare
A Clearer Path to Smarter Self-Insurance
We’re Vālenz Health®, your partner in improving health literacy, reducing plan spend, and delivering high-value healthcare. Valenz means strong, vigorous, and healthy—traits that define us and the results we deliver.
What that means for you: an industry-leading team that tackles your biggest challenges throughout the patient healthcare journey.

One Integrated Platform for Simplified Self-Funding
Your Destination to Optimize Healthcare
When you’re stuck managing the chaos of self-insurance, you have no focus left for what really matters—engaging your members and containing costs.
Valenz is here to help. As the leading platform of integrated self-insurance solutions, we’re the single destination for patients, payers, plans, and providers to reduce costs, improve quality, and optimize the entire healthcare experience.
When Healthcare Works as ONE, Everyone Wins
ValenzONE is a health plan optimizer that integrates cost containment and member engagement—connecting members with high-quality, lower-cost providers and health systems to deliver measurable savings.
Built for the future of self-funded benefits, ValenzONE replaces outdated financial models with transparent, variable copays tied to provider value.
The result? Empowered members, improved outcomes, and 7%-12% average employer savings across the board.
Drive Better Health Outcomes
Turning Complexity Into Clarity
Give your health plan members the data-driven tools they need to make confident healthcare choices.
Our fully integrated suite of solutions demystifies the healthcare process, delivering higher-value care and reducing plan spend.
It's all a part of our mission: to optimize the utilization of high-value healthcare to protect the patient and the employer.

Whatever Your Role, Let's Simplify It
Smarter, Better, Faster Healthcare Starts Here
Learn how Valenz can meet your health plan needs, no matter who you are.
Proven Performance, Powerful Stories
Health Plan Management Group
"Thanks to the robust front-end care navigation solution, Valenz unlocked the true value of [our client's] new plan — members are now guided to high-quality, in-network providers."
Health Plan Member
“Love it! With our new plan, not only are my out-of-pocket costs lower, but filling my specialty drug prescriptions is so much easier."
Valenz Maternity Case Manager
“The new mom appreciated the support and was grateful to have prevented unnecessary out-of-pocket costs for the NICU. Her employer was grateful for the cost-savings, too — and for our help in making it possible for their employee and her baby to live strong, vigorous, and healthy lives.”
Manage Costs through the Entire Patient Journey
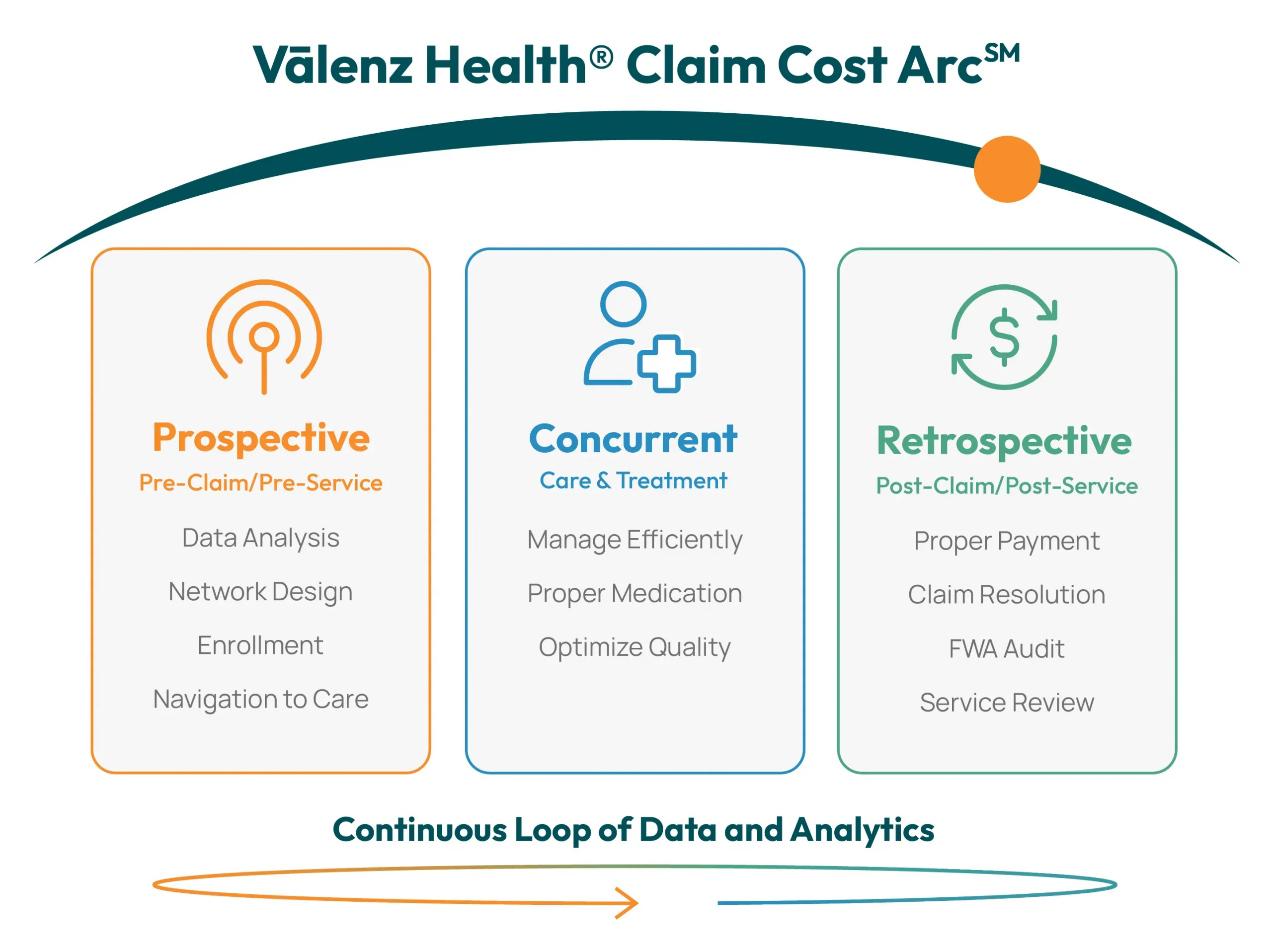
Engage Early and Often Across the Claim Cost ArcSM
Address your health plan needs with Valenz. By combining data-driven insights with innovative solutions, we allow payers to manage their costs across each phase of the patient journey.
See How Much Your Plan Can Save
Reduce your health plan spend with Valenz as your partner. Discover your savings potential by contacting our team today.
Explore Our Latest Thinking
Timely Updates and Industry Insights That Matter
Address your health plan needs with confidence and clarity by staying current on the latest industry developments. Check out our resources for insights, news coverage, event appearances, and more.
Ready to Simplify Self-Insurance?
Your Journey Starts Here
Connect with a Valenz team member to explore the difference our solutions can make for you.