Link to: Vālenz<sup>®</sup> Health Acquires KISx Card, LLC, Enhancing Solutions for High-Cost Surgical and Imaging Procedures
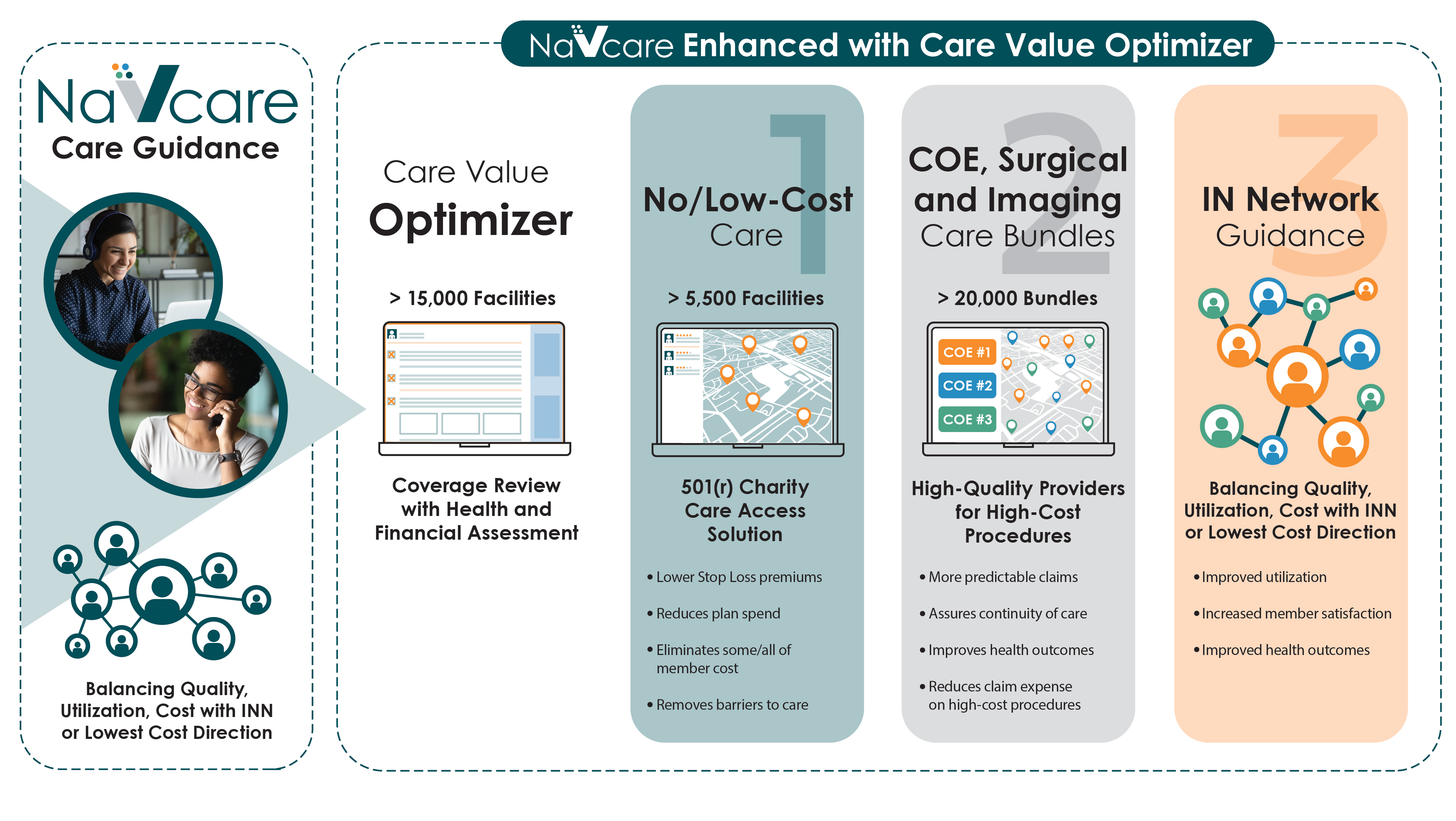
Care Value Optimizer
Delivering navigated access to high quality, lower cost care
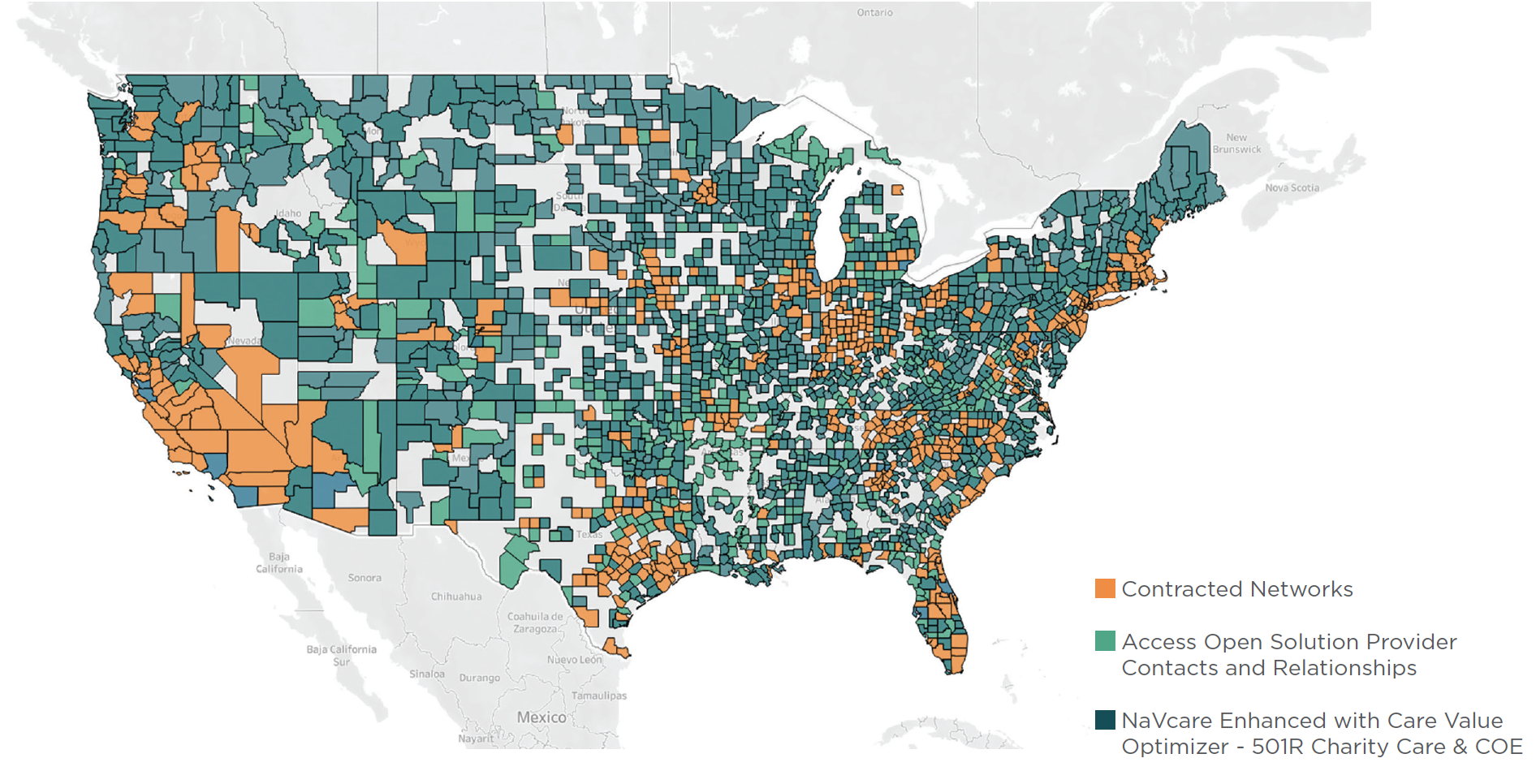
Self-insured plans finally have a solution that triages network selection, care and treatment based on both the financial and health needs of the member: NaVcare Enhanced with Care Value Optimizer, a data-enabled tool used by Vālenz® Health nurse navigators to swiftly identify the best available care options based on members’ income, location and healthcare needs. We tailor care to each member, matching members to high-quality providers and provider networks – from low-cost and no-cost charity care options to Centers of Excellence (COE), imaging, and surgical care bundles. Our care guidance balances quality, utilization and cost with an emphasis on keeping members in-network at the highest possible level of quality care for the lowest cost.
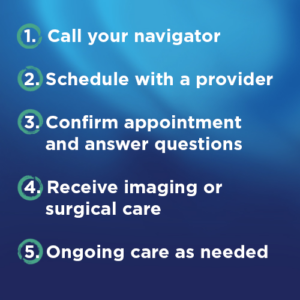
How Enhanced Care Navigation Works
- When members have a care need, they call (800) 441-7705 to engage with a NaVcare team member.
- If the member is a match for a low-cost/no-cost opportunity, the navigator facilitates the necessary paperwork, scheduling, and selection of a provider prior to care.
- If the member is not a match, the navigator evaluates our Centers of Excellence which cover thousands of procedures – including imaging and surgical care – from high-quality providers across all 50 states.
- If neither of the above is a good match, nurses navigate the member to in-network options. Only as a last resort will the navigator select an out-of-network solution.
- All levels are wrapped with our Care Management services to ensure best value and continuity of care.
Centers of Excellence, Surgical and Imaging Bundles
Access 20,000 Care Bundles
Member benefits:
- High quality providers for high-cost procedures, including imaging and surgical care
- Improves health outcomes
- Assures continuity of care
Employer benefits:
- Reduces claim expense on high-cost procedures
- Improves overall member experience
Care Bundles from Top Centers of Excellence
Access the nation’s top health facilities and hospitals to manage the most costly and complex procedures and treatments with Centers of Excellence care bundles:
- Addiction Treatment
- Bariatric Surgery
- Behavioral Health
- Cardiovascular
- Complex Cancer
- Ear, Nose & Throat
- Executive Health
- Gastroenterology
- Gender Affirmation
- Gene Therapy
- Imaging
- Neurosurgery
- Obstetrics & Gynecology
- Ophthalmology
- Orthopedics
In Network Provider Direction
Access In Network Providers: 70,000
Member benefits:
- Improves health outcomes
- Enhances member satisfaction
Employer benefits:
- Balance quality, utilization and cost
- Drive cost savings with in network care