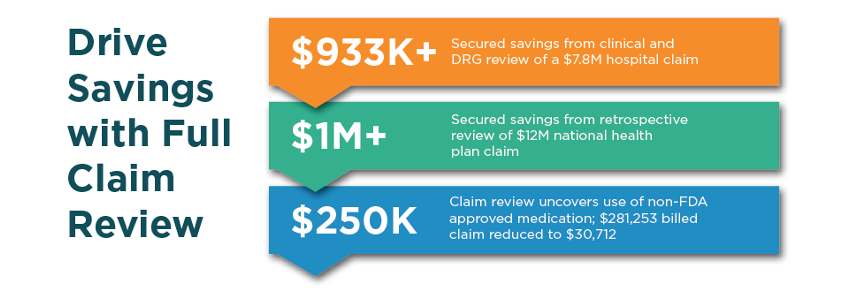
Secured Savings with Full Claim Review
With payment errors or overpayments expected to cost up to $560 billion, or 7-10% of healthcare spending in 2026, payers need solutions that maximize savings on every claim, regardless of type or size. That’s why Vālenz® Health through its suite of Validation, Integrity and Accuracy (VIA) Solutions offers ProteKHt™ full claim review.
Designed to eliminate erroneous, questionable billing charges and unnecessary charges associated with fraud, waste and abuse, ProteKHt ensures appropriate, defensible and transparent payments secured by signed provider agreements. In fact, our customers experience signoff success rates averaging 70%, with less than 5% of reviews overturned by providers.