https://www.valenzhealth.com/wp-content/uploads/2024/04/Valenz_Srini-Annc_600x432-v2-.jpg
432
600
Jessica Lahasky
https://www.valenzhealth.com/wp-content/uploads/2023/01/valenz-logo-1-23-3.png
Jessica Lahasky2024-04-19 14:56:362024-04-19 19:01:00Srinivas Achukola Joins Vālenz® Health as New Chief Information Officer
https://www.valenzhealth.com/wp-content/uploads/2024/04/Valenz_Srini-Annc_600x432-v2-.jpg
432
600
Jessica Lahasky
https://www.valenzhealth.com/wp-content/uploads/2023/01/valenz-logo-1-23-3.png
Jessica Lahasky2024-04-19 14:56:362024-04-19 19:01:00Srinivas Achukola Joins Vālenz® Health as New Chief Information OfficerVālenz® Care for Taft-Hartley Trusts
Empower members to take charge of their health – for better outcomes and significant cost containment.
Vālenz® Care offers a suite of triple URAC-accredited care management services for Taft-Hartley Funds and Trusts, including multi-employer groups, associations and public entities, targeting the most appropriate levels of care at the beginning of the patient journey. Through our concierge-level member care navigation, we offer a smarter way to manage health administrative costs while ensuring a high quality of care.
Lower healthcare costs require highly sophisticated and comprehensive care management strategies, which are particularly important for Taft-Hartley Funds and Trusts:
- Unionized workers often negotiate for a comprehensive package of health benefits, so Funds must find effective ways to keep healthcare contribution rates down.
- Collective bargaining allows unions to extend coverage into retirement, so understanding how to manage care and costs for this population as they age is critical.
We provide your organization – and your workforce – with the right data-driven tools and care-optimized solutions for proactive health management. Position yourself to succeed in population health initiatives and medical cost management by connecting the clinical dots with Valenz Care.
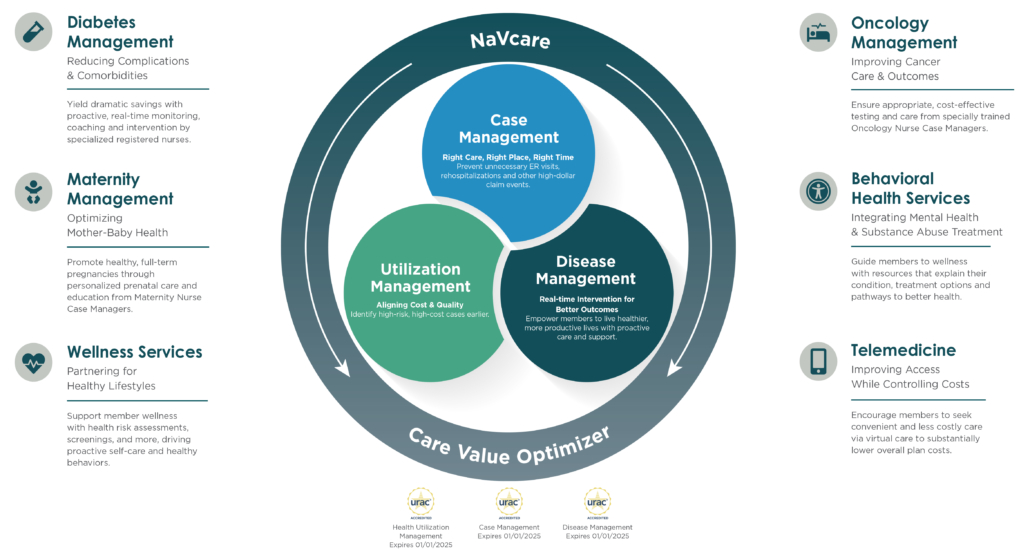
Utilization Management
Facilitates early identification of high-risk, high-cost cases, prevents rehospitalization and reduces costs.
Case Management
Improves quality of care while steering members to network providers and maximizing cost savings.
Disease Management
Combats chronic illness, reduces costs and helps members live healthier, more productive lives.
Vālenz Care helps build a healthy, thriving workforce by ensuring the right care in the right place at the right time – every time. We achieve this by integrating our high-value provider networks and care management services with data-driven claim and compliance solutions in our comprehensive Health Ecosystem Optimization Platform.
As the foundation of our commitment to clinical and member advocacy, Valenz Care engages early and often to deliver triple URAC-accredited services for case management, disease management and utilization management. We manage high-cost medical care more effectively through the Care Value Optimizer, without compromising on the quality of care.
Traditionally, a small number of claims, just 5-15% of claims, represent up to 70% of an employer’s health spend. The CVO changes this paradigm. Utilizing NaVcare, Valenz ensures a high-quality health outcome at the best price, by navigating through the myriad of care options for high-cost surgical procedures while controlling costs along the way.
First, we determine if the patient qualifies for no cost or low-cost options. Often overlooked, patients living at or below 400% of the federal poverty level can quality for full or partial elimination of bills, deductibles and copays. For those not qualifying, we offer Center of Excellence bundles for a host of high-cost procedures. Identifying high-quality ASCs and hospital centers with best-in-class outcomes, we find the right facility for the patient’s unique needs in a way that is far cheaper than traditional healthcare networks.
Ultimately, we enable your population to shift from reactive care to proactive, interactive health management – significantly reducing plan costs and driving improved health and wellness for your workforce. See what Valenz Care can do for Taft-Hartley Trusts, associations and public entities to drive smarter, better, faster healthcare.
NaVcare
NaVcare empowers individuals to make better health decisions while controlling costs, improving outcomes and enhancing the experience. Working one-on-one with plan members, our care navigators deliver personalized, concierge-level guidance through each step of the patient journey.
Integrated virtual care
Valenz Care includes seamlessly integrated virtual care services. Your plan members have 24/7 access to board-certified physician care, minimizing your exposure to unnecessary ER visits and health risks while contributing to improved patient outcomes.
“I wanted to thank my nurse case manager for her advice and support through a very difficult time for me and my family. She provided great information and helped coordinate my care!”
– Jenn S., plan member
Experience the Synergy
When we say the Valenz ecosystem is comprehensive, we mean it. With a complete selection of fully integrated wraparound solutions to complement the core solutions featured below, we deliver benefits far greater than the sum of all these parts individually.
Vālenz Access
Combine a quality-first provider network or open solution with a range of customized, data-driven services from the Access Solutions Suite.
Vālenz Care
Guide members to better care and outcomes at lower costs, for you and for them, with RN-led, triple URAC-accredited care management.
Vālenz Claim
Reduce costs and ensure accurate payments with comprehensive bill reviews and repricing methodologies, integrated analytics, and more.
Vālenz Assurance
Improve coding, reimbursement assurance, auditing, claim accuracy and compliance monitoring, all while saving time and costs.
v-Lens
Use advanced, drill-down analytics and predictive modeling to continuously disrupt the cost curve without compromising quality.